Small Intestinal Bacterial Overgrowth (SIBO) often results from impaired gut motility, specifically dysfunction in the Migrating Motor Complex (MMC). This natural "cleansing wave" prevents bacterial buildup in the small intestine. Without proper motility, bacteria ferment leftover food, causing bloating, nutrient malabsorption, and other symptoms. While antibiotics can temporarily reduce bacterial overgrowth, nearly 45% of patients experience relapse due to unresolved motility issues.
Key approaches to improving gut motility for SIBO include:
- Prebiotics: Non-digestible fibers like inulin and FOS stimulate gut contractions by producing short-chain fatty acids (SCFAs). They also support beneficial bacteria but may initially cause bloating.
- Probiotics: Live microorganisms regulate gut motility by interacting with the nervous system and releasing neurotransmitters like serotonin. However, some strains may worsen symptoms for certain individuals.
- Postbiotics: Non-living microbial components, such as SCFAs and tryptophan metabolites, enhance motility without the risks associated with live bacteria.
A combined approach, such as synbiotics (prebiotics + probiotics), has shown promising results, with studies reporting a 93.3% success rate in eradicating SIBO compared to 66.7% with antibiotics alone. Products like Begin Rebirth RE-1™ offer targeted solutions by integrating prebiotics, probiotics, and postbiotics to restore motility and reduce recurrence.
While these interventions show potential, individual responses vary, and starting with low doses can help minimize side effects. Long-term management requires addressing the root cause - impaired motility - to break the cycle of SIBO relapse.
SIBO and IMO: Understanding Gut Overgrowth, Methane, and Archaea
1. Prebiotics
Prebiotics are non-digestible fibers like inulin, fructooligosaccharides (FOS), and galactooligosaccharides (GOS) that serve as food for beneficial gut bacteria such as Bifidobacterium and Lactobacillus. When fermented, these fibers produce short-chain fatty acids (SCFAs) like acetate, butyrate, and propionate. These SCFAs play a key role in stimulating smooth muscle contractions, which helps speed up gastrointestinal transit [8].
In addition to SCFA production, inulin-type prebiotics help counter oxidative stress and offer protection to the colonic mucosa [7]. Dr. Małgorzata Grembecka from the Medical University of Gdańsk explains:
Prebiotics accelerate gut motility via the gut-brain axis and bacteria metabolites [2].
The benefits of prebiotics are particularly evident in cases of small intestinal bacterial overgrowth (SIBO). A 2014 study showed that 93.3% of SIBO patients who used a synbiotic treatment (Bacillus coagulans combined with FOS) achieved a negative breath test and complete pain relief. This was significantly better than the results seen in the antibiotic-only group, which had success rates of 66.7% and 46.7%, respectively [4].
For improved motility, effective dosages include 2.5–5 g/day of inulin, 10 g/day or more of FOS, and 1–3 g/day of lactulose [7]. However, starting with high doses can sometimes cause mild bloating that resembles SIBO symptoms. Additionally, excessive amounts of FOS or GOS may temporarily lower butyrate-producing bacteria, as the resulting increase in lactic acid creates an unfavorable environment for those strains [7]. To avoid these issues, it’s best to begin with a low dose, such as 2.5 g of inulin, and gradually increase it, ideally after addressing SIBO. Consistency is key - benefits may fade within just seven days of stopping prebiotic intake, underscoring the importance of long-term use [7].
2. Probiotics
Probiotics are live microorganisms that play a key role in supporting gut health. They help regulate gut motility by directly stimulating the enteric nervous system (ENS) and interstitial cells of Cajal (ICC) - the gut's natural pacemakers. Additionally, they trigger the release of neurotransmitters like serotonin, Substance P, and ghrelin, which are essential for driving peristalsis. Probiotics also produce short-chain fatty acids that stimulate enteroendocrine cells to release GLP-1 and peptide YY, further influencing motor responses in the gut [5].
Clinical studies highlight the potential of probiotics in managing small intestinal bacterial overgrowth (SIBO). For example, a meta-analysis revealed that probiotics achieved a 62.8% decontamination rate and reduced hydrogen levels in breath tests by an average of 36.35 ppm [9]. In a six-month study, a combination of Bacillus coagulans and fructooligosaccharides (FOS) led to a 93.3% rate of negative breath tests, compared to 66.7% with antibiotics alone. Moreover, 100% of patients in the probiotic group experienced complete abdominal pain resolution, compared to just 46.7% in the antibiotic-only group [4].
Dr. Wei Chung Chen and Dr. Eamonn MM Quigley from Houston Methodist Hospital noted:
"The inclusion of the synbiotic augmented the clinical impact of the antibiotic and may have increased the likelihood of eradication of SIBO" [4].
However, there are limitations to consider. Many probiotic strategies for SIBO rely on empirical evidence rather than large-scale clinical trials, and outcomes can vary significantly based on factors like probiotic strains, patient demographics, and diagnostic methods [4]. In rare cases, patients with short bowel syndrome may experience excessive Lactobacillus growth, which can lead to d-lactic acidosis and neurological symptoms such as confusion and slurred speech [3].
Since SIBO often stems from underlying motility disorders, probiotics should be part of a broader treatment plan. While the benefits are promising, understanding their nuanced effects and potential risks underscores the importance of a comprehensive and well-rounded approach to treatment. This topic will be further explored in the next section focusing on specific products.
3. Postbiotics
Postbiotics are non-living microbial components - like metabolites, cell fragments, or bioactive compounds - that can provide health benefits. They also tend to have better safety and stability during storage and shipping compared to live probiotics [13][14].
When it comes to gut motility, postbiotics work in fascinating ways. For instance, short-chain fatty acids (SCFAs) like butyrate interact with the enteric nervous system to help regulate intestinal contractions. Tryptophan, a precursor to serotonin, speeds up transit time and aids in gastric emptying [2]. Unlike prebiotics, which rely on fermentation within the gut to produce these effects, postbiotics deliver these compounds in a more controlled manner, reducing the risk of fermentation-related side effects. Additionally, cell-free extracts from E. coli Nissle have been shown to stimulate the contractility of colonic smooth muscles, while also supporting tight junction proteins to address "leaky gut" symptoms [10].
Clinical research backs up the benefits of postbiotics. In 2019, a study led by Nishida et al. found that heat-inactivated L. gasseri CP2305 reduced anxiety and sleep disturbances while also shortening the time it took participants to fall asleep. This highlights how even non-viable microbes can positively influence the gut-brain connection [12]. Another study by Depommier et al. demonstrated that pasteurized Akkermansia muciniphila improved insulin sensitivity and reduced markers of liver dysfunction and inflammation [12]. Despite these promising results, there are some challenges to consider.
In the small intestine, SCFAs can activate the "ileal brake", which releases hormones like PYY, neurotensin, and GLP-1. While this mechanism slows motility to prevent bacterial overgrowth, it may also promote bacterial stasis [11]. For individuals with short bowel syndrome, postbiotic fermentation could lead to D-lactic acidosis, a condition that can cause neurological symptoms [1]. Elevated serum folic acid - another fermentation byproduct - has been linked to small intestinal bacterial overgrowth (SIBO). For example, in patients with chronic pancreatitis and SIBO, serum folic acid levels were significantly higher (16.5 ng/dL) compared to those without SIBO (8.32 ng/dL). A strong correlation (r = 0.637, p = 0.002) was observed in cases of methane-dominant SIBO [10].
Postbiotics offer a promising tool for managing SIBO by improving gut motility and stability, especially for individuals prone to fermentation-related issues. Their safety and stability make them a valuable addition to strategies aimed at addressing impaired gut function in SIBO [13].
sbb-itb-1bbfe7f
4. Begin Rebirth RE-1™
Mechanism of Action
Begin Rebirth RE-1™ brings together prebiotics, probiotics, and postbiotics into a single, targeted solution aimed at improving gut motility in individuals with SIBO. Its carefully designed formula includes a 4.5 g fiber blend of GOS and inulin, which promotes the production of short-chain fatty acids (SCFAs). These SCFAs play a key role in stimulating the gut–brain axis, speeding up transit time, and encouraging colonic smooth muscle contractions [2] [8].
The probiotic component, powered by Human Origin Strains (HOSt™) delivering 500 billion CFU per serving, helps regulate neural-dependent motility reflexes while competing against harmful bacteria [2] [4]. Meanwhile, the postbiotic fraction provides butyrate, which supports smooth muscle contractions and lowers intestinal pH, creating an environment less favorable for bacterial overgrowth [8].
Thanks to the Lyosublime™ system, absorption is optimized without requiring refrigeration. The formulation is designed to target the Migrating Motor Complex (MMC) - a critical mechanism that clears food residue and bacteria from the small intestine. This is particularly important since approximately 45% of patients experience SIBO recurrence after antibiotic treatment [1]. To address varying needs, the product offers flexible reset protocols of 7 days, 4 weeks, or 12 weeks.
Efficacy in SIBO Motility
The approach behind Begin Rebirth RE-1™ aligns with clinical findings, which highlight the effectiveness of synbiotic therapy in improving gut motility. Studies report up to 93.3% of patients achieving negative breath test results and complete pain resolution, emphasizing its potential to enhance small bowel transit time (SBTT) [4]. Research also reveals that nearly half of SIBO patients (47.6%) experience an SBTT of 6 hours or longer, compared to a healthier average of about 4.2 hours [15]. By restoring MMC function and accelerating transit, synbiotics help combat bacterial stasis, a key factor in overgrowth. Evidence supports that the combination of prebiotics, probiotics, and postbiotics can significantly reduce colonic transit time, boost bowel movement frequency, and improve stool consistency better than single-strain treatments [8].
Potential Limitations
While Begin Rebirth RE-1™ offers many benefits, some users may experience mild fermentation-related symptoms initially due to the prebiotic fibers. To minimize these effects, starting with a lower dose or opting for a shorter reset protocol can be helpful. Gradually increasing the dosage allows for smoother adaptation and supports long-term improvements in gut motility.
Pros and Cons
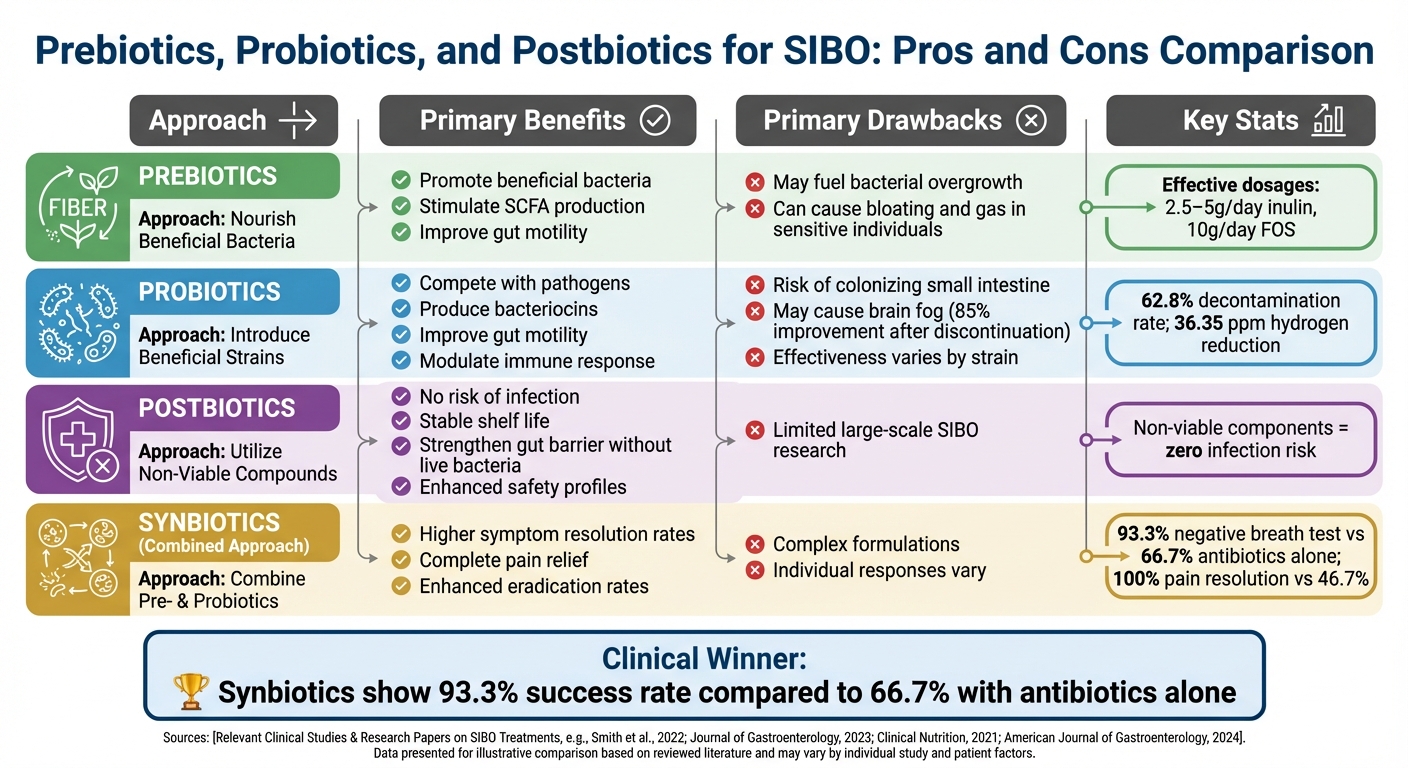
Prebiotics vs Probiotics vs Postbiotics for SIBO Treatment Comparison
Let’s break down the advantages and disadvantages of prebiotics, probiotics, and postbiotics when it comes to treating SIBO (Small Intestinal Bacterial Overgrowth). The following table provides a clear summary of these points.
Prebiotics are known to encourage the production of short-chain fatty acids (SCFAs) and improve gut motility. However, they can aggravate bacterial overgrowth in the small intestine, leading to uncomfortable symptoms like gas and bloating if the underlying overgrowth isn’t addressed first [4][16].
Probiotics work by introducing beneficial bacterial strains that compete with harmful pathogens. But there’s a catch: according to Dr. Rao, probiotics can sometimes colonize the small intestine, potentially worsening SIBO symptoms and even causing brain fog [16]. In fact, one study revealed that 85% of SIBO patients experiencing brain fog saw complete improvement after discontinuing probiotics and starting antibiotics [16].
Postbiotics, on the other hand, provide a safer option. These contain non-living microbial components, which eliminates the risk of infection or bacterial translocation. As Sylwia Smolinska from the Department of Clinical Immunology explains:
"Postbiotics offer non-viable microbial components and metabolites that mimic probiotic benefits with enhanced safety profiles" [6].
The downside? Large-scale studies specifically focusing on SIBO are still limited [6].
Here’s a concise comparison of the pros and cons for these approaches:
| Approach | Primary Benefits | Primary Drawbacks |
|---|---|---|
| Prebiotics | Promote beneficial bacteria; stimulate SCFA production [2][6] | May fuel bacterial overgrowth; can cause bloating and gas in sensitive individuals [4][16] |
| Probiotics | Compete with pathogens; produce bacteriocins; improve gut motility; modulate immune response [4][6] | Risk of colonizing the small intestine; may cause brain fog; effectiveness varies by strain [6][16] |
| Postbiotics | No risk of infection; stable shelf life; strengthen gut barrier without live bacteria [6] | Limited research on large-scale SIBO trials [6] |
| Synbiotics | Higher symptom resolution rates; 93.3% negative breath test compared to 66.7% with antibiotics alone [4] | Formulations can be complex; individual responses depend on gut conditions [4] |
Each option comes with its own set of strengths and challenges, making it important to tailor treatments to individual needs and conditions.
Conclusion
Taking a synbiotic approach has proven to be an effective way to manage SIBO and improve gut motility. One clinical study highlighted this by showing that a synbiotic regimen achieved a 93.3% negative hydrogen breath test rate, compared to 66.7% with antibiotics alone. Even more compelling, all patients in the synbiotic group experienced full relief from abdominal pain, while only 7 out of 15 patients (around 47%) in the antibiotic-only group reported similar results [4].
While individual biotics like Lactobacillus reuteri can be useful for short-term, targeted interventions - such as modulating neural-dependent motility reflexes [2] - long-term management calls for a more comprehensive solution. Begin Rebirth RE-1™ steps up to this challenge with its 3-in-1 formulation that combines prebiotics, probiotics, and postbiotics. Each serving delivers 500 billion CFU, includes Human Origin Strains (HOSt™), and utilizes the Lyosublime™ delivery system to ensure optimal absorption without the need for refrigeration. This formulation works to address the underlying motility dysfunction that often leads to SIBO recurrence, offering a pathway to more sustained outcomes.
Using integrated formulations like these for ongoing maintenance and prevention is key to breaking the cycle of SIBO relapse and incomplete symptom relief. As Wei Chung Chen and Eamonn MM Quigley from Houston Methodist Hospital noted:
"The inclusion of the synbiotic augmented the clinical impact of the antibiotic and may have increased the likelihood of eradication of SIBO" [4].
A 3-in-1 synbiotic formulation like Begin Rebirth RE-1™ offers a targeted and effective way to achieve lasting relief from SIBO while improving gut motility for better overall digestive health.
FAQs
How do prebiotics and probiotics help improve gut motility in SIBO?
Prebiotics and probiotics are essential for improving gut motility, a function that’s often compromised in small intestinal bacterial overgrowth (SIBO). Prebiotics, which are fermentable fibers, serve as food for beneficial gut bacteria. These bacteria produce short-chain fatty acids (SCFAs) and other compounds that trigger the release of hormones like motilin and serotonin. These hormones play a key role in activating the migrating motor complex (MMC), which keeps the intestines moving smoothly and prevents stagnation - a condition that can lead to bacterial overgrowth.
Probiotics, on the other hand, introduce live beneficial bacteria into the gut. These bacteria work in several ways to support motility: they compete with harmful microbes, produce bioactive compounds that regulate muscle contractions, and interact with the enteric nervous system to help restore proper MMC activity. When used together, prebiotics and probiotics create a healthier gut environment, improving motility and easing symptoms like bloating and constipation that are common with SIBO.
For a more complete solution to gut health, products like Begin Rebirth RE‑1™ combine prebiotics, probiotics, and postbiotics to help reset the microbiome and support optimal intestinal function.
What side effects can prebiotics and probiotics cause for people with SIBO?
Prebiotics and probiotics are generally safe for most people, but if you have Small Intestinal Bacterial Overgrowth (SIBO), they might lead to temporary digestive discomfort. Common side effects include bloating, gas, abdominal pain, and changes in bowel movements, such as diarrhea or constipation. These reactions often happen as your gut adjusts to the introduction of new microbes or fermentable fibers.
Prebiotics, particularly high-FODMAP fibers, can sometimes aggravate symptoms by providing fuel for the excess bacteria in the small intestine. Probiotics, on the other hand, might temporarily disrupt the microbial balance, causing mild discomfort. The good news is that these effects typically subside within a few days to weeks as your gut gets used to the changes. To reduce these issues, it’s crucial to choose specific strains and dosages that align with SIBO management needs.
Why are postbiotics considered a safer choice for managing SIBO?
Postbiotics, the non-living byproducts of microbial activity, provide health benefits without the potential concerns that come with introducing live bacteria into the gut. This makes them a safer choice for those dealing with Small Intestinal Bacterial Overgrowth (SIBO), as they don’t risk worsening bacterial overgrowth.
By improving gut health and calming inflammation without increasing bacterial levels, postbiotics can help manage SIBO symptoms. They also support better gut motility and contribute to maintaining overall digestive balance.

