Your gut health relies heavily on the interaction between micronutrients and the trillions of bacteria living in your digestive system. Here's the key takeaway: combining specific vitamins and minerals doesn't just support your gut - it amplifies their effects, improving nutrient absorption, bacterial diversity, and overall gut function.
Key Insights:
- Gut bacteria produce 40%-65% of essential B-vitamins like biotin, folate, and riboflavin.
- Deficiencies in vitamin A, zinc, or iron disrupt gut balance, altering bacterial populations and gene expression.
-
Nutrient combinations work better together:
- Vitamin D needs magnesium to activate and influences gut bacteria like Bifidobacterium and Faecalibacterium.
- Zinc and vitamin A strengthen the gut barrier and regulate bacterial diversity.
- B-vitamins fuel short-chain fatty acid (SCFA) production, crucial for gut health.
Clinical Evidence:
- A 2025 clinical trial showed a 49-fold increase in Urolithin A, a key gut metabolite, when probiotics were paired with polyphenols.
- Zinc paired with probiotics like Lactobacillus plantarum significantly improved zinc absorption.
Practical Tips:
- Pair zinc-rich foods (like oysters) with probiotics (yogurt, kimchi) to boost absorption.
- Combine magnesium (nuts, greens) with vitamin D for better gut health.
- Include polyphenol-rich foods (pomegranate, berries) to support beneficial bacteria.
These findings highlight the importance of nutrient synergy in maintaining a healthy gut microbiome and improving overall health.
How Micronutrient Combinations Affect Gut Bacteria
Certain vitamins and minerals don’t just work in isolation; they often team up, creating combined effects that influence the gut microbiome. These nutrients interact through specific biochemical pathways, shaping the balance and diversity of gut bacteria.
Vitamin D and Magnesium
When it comes to vitamin D, magnesium plays a key supporting role. Magnesium acts as a cofactor, helping activate vitamin D. Without enough magnesium, vitamin D can’t do its job. Even more interesting, magnesium encourages gut bacteria to assist in vitamin D synthesis.
For example, in the Personalized Prevention of Colorectal Cancer Trial (NCT04229992), 226 participants showed notable changes in their gut bacteria when magnesium was added to their diets. Researchers observed a 23.01% increase in Carnobacterium maltaromaticum and a 2.13% rise in Faecalibacterium prausnitzii among individuals with proper TRPM7 function[7]. These bacteria are known to play a role in vitamin D production. Another study found that taking 4,000 IU of vitamin D₃ over 12 weeks enriched gut bacteria from the Bifidobacteriaceae family in healthy adults[9]. And when vitamin D₃ was paired with probiotics like Lactobacillus and Bifidobacterium strains, a review of seven clinical trials showed improvements in metabolic health and reduced disease severity in patients with gestational diabetes and PCOS over 6–12 weeks[8].
Zinc and Vitamin A
Zinc and vitamin A form another powerful duo for gut health. Vitamin A aids in producing mucin (a protective layer for the gut lining) and supports cell differentiation, while zinc strengthens the tight junctions between intestinal cells, keeping the gut barrier intact. A deficiency in either nutrient can weaken the gut’s defenses, allowing harmful bacteria to thrive.
Research from Washington University School of Medicine in 2017 highlighted how vitamin A deficiency can disrupt gut bacteria. In gnotobiotic mice, a lack of vitamin A led to a significant increase in Bacteroides vulgatus, but retinol treatment helped regulate this imbalance through the AcrAB-TolC efflux system[4]. Similarly, a 2016 study of Chinese infants with persistent diarrhea linked low vitamin A levels (serum retinol <0.7 µmol/L) to reduced microbial diversity and a 50% spike in Enterococcaceae, including Enterococcus faecalis[12]. In children with autism spectrum disorders, a single high dose of vitamin A reduced Enterobacter and Clostridium populations by 94% and Escherichia-Shigella by 51%[12]. Zinc, on the other hand, has been shown to improve microbial diversity and lower inflammation when paired with probiotics like Lactobacillus plantarum[5].
B-Vitamins and Short-Chain Fatty Acid Production
B-vitamins are essential for gut bacteria to produce short-chain fatty acids (SCFAs), such as butyrate, which are crucial for gut health. These vitamins serve as cofactors in the chemical reactions that drive SCFA production.
Take thiamine (B₁), for instance - it helps convert pyruvate into acetyl-CoA, a critical step in butyrate production[13][10]. Riboflavin (B₂) is another key player, working within the electron transfer flavoprotein complex to aid in butyrate synthesis[13][10]. Niacin (B₃) also contributes by boosting acetate production, which helps maintain gut balance[10].
"Butyrate production directly depends on the presence of two vitamins: thiamine is a cofactor of pyruvate:ferredoxin 2-oxidoreductase... and riboflavin is part of the electron transfer flavoprotein complex with butyryl-CoA dehydrogenase." – mBio Journal[13]
Interestingly, many butyrate-producing bacteria, like Faecalibacterium prausnitzii and Roseburia species, can’t make these vitamins on their own. Instead, they rely on dietary intake or cross-feeding from other bacteria. Research shows that most Roseburia species and Eubacterium rectale strains depend on folate (B₉) and thiamine (B₁)[13]. In fact, around 20–30% of gut bacteria species lack the ability to produce at least one essential B-vitamin[11][2]. This highlights how crucial it is to get enough B-vitamins through diet to support these beneficial bacteria, which, in turn, help maintain gut health by strengthening the gut barrier and reducing inflammation.
How Micronutrient Combinations Work in the Gut
Improved Nutrient Absorption
Micronutrients often rely on one another to be absorbed and utilized effectively. Take magnesium, for example - it’s a vital cofactor for enzymes that process vitamin D. Without enough magnesium, vitamin D can’t perform at its best, limiting its benefits [5]. Similarly, the absorption of vitamin A in the small intestine, which typically ranges between 70% and 90%, depends on a healthy gut barrier [12].
The gut microbiome also plays a key role in nutrient absorption. Certain gut bacteria release enzymes called phytases that break down phytic acid, freeing up minerals like calcium, magnesium, iron, and phosphorus [5]. Additionally, when gut bacteria ferment dietary fiber, they produce short-chain fatty acids (SCFAs). These SCFAs lower the pH in the gastrointestinal tract, improving the solubility and absorption of minerals [5].
There’s even evidence from clinical trials showing that pairing zinc with specific probiotics can boost its absorption. For instance, when zinc is taken alongside Lactobacillus plantarum, blood zinc levels increase more significantly than when zinc is consumed on its own [5]. This highlights how the gut microbiome works in tandem with nutrients to optimize absorption.
How Gut Bacteria Use Nutrients
The gut is home to two main types of bacteria: prototrophs (producers) and auxotrophs (consumers). Prototrophs can create B-vitamins from scratch and share them with auxotrophs, which lack the ability to produce these vitamins. This sharing system, known as syntrophic cross-feeding, ensures that the microbial community remains stable, even when dietary intake of B-vitamins is low [2][11]. In fact, about 20–30% of gut bacteria depend on external sources of B-vitamins [11].
"B-vitamin sharing promotes stability of gut microbial communities... revealing a remarkable stability with respect to widely varying levels of exogenously supplied micronutrients." – Vandana Sharma, Infectious and Inflammatory Disease Center, Sanford Burnham Prebys Medical Discovery Institute [11]
Gut bacteria don’t just share nutrients - they also transform them to make them more effective. For example, Lactobacillus fermentum converts Fe(III) into the more absorbable Fe(II) [3]. Similarly, Escherichia coli uses an enzyme called CurA to convert curcumin into tetrahydrocurcumin, which has better bioavailability and neuroprotective properties [14]. Human gut microbes are also responsible for producing a significant portion - between 40% and 65% - of essential B-vitamins like biotin, folate, and riboflavin [5]. These transformations highlight the dynamic and vital role of gut bacteria in nutrient utilization.
Gut Barrier Protection
Micronutrients do more than just support absorption - they also help protect the gut barrier. For example, vitamin A plays a critical role in producing mucin, the protective layer that lines the gut, and aids in proper epithelial cell differentiation. A lack of vitamin A can weaken this barrier, leaving the gut more vulnerable [12][4]. Vitamin D complements this by promoting the production of antimicrobial peptides and proteins, which help maintain the integrity of tight junctions between intestinal cells [5][12].
SCFAs, produced during the fermentation of dietary fiber, also play a role in strengthening the intestinal barrier by supporting colonocyte function and reducing inflammation [5]. Research using gnotobiotic models has shown that vitamin A deficiency has a greater impact on the structure and function of the gut microbiome than deficiencies in folate, iron, or zinc [4]. This demonstrates how specific nutrient combinations can help maintain gut health and prevent imbalances in the microbial community, also known as dysbiosis.
What Recent Studies Show
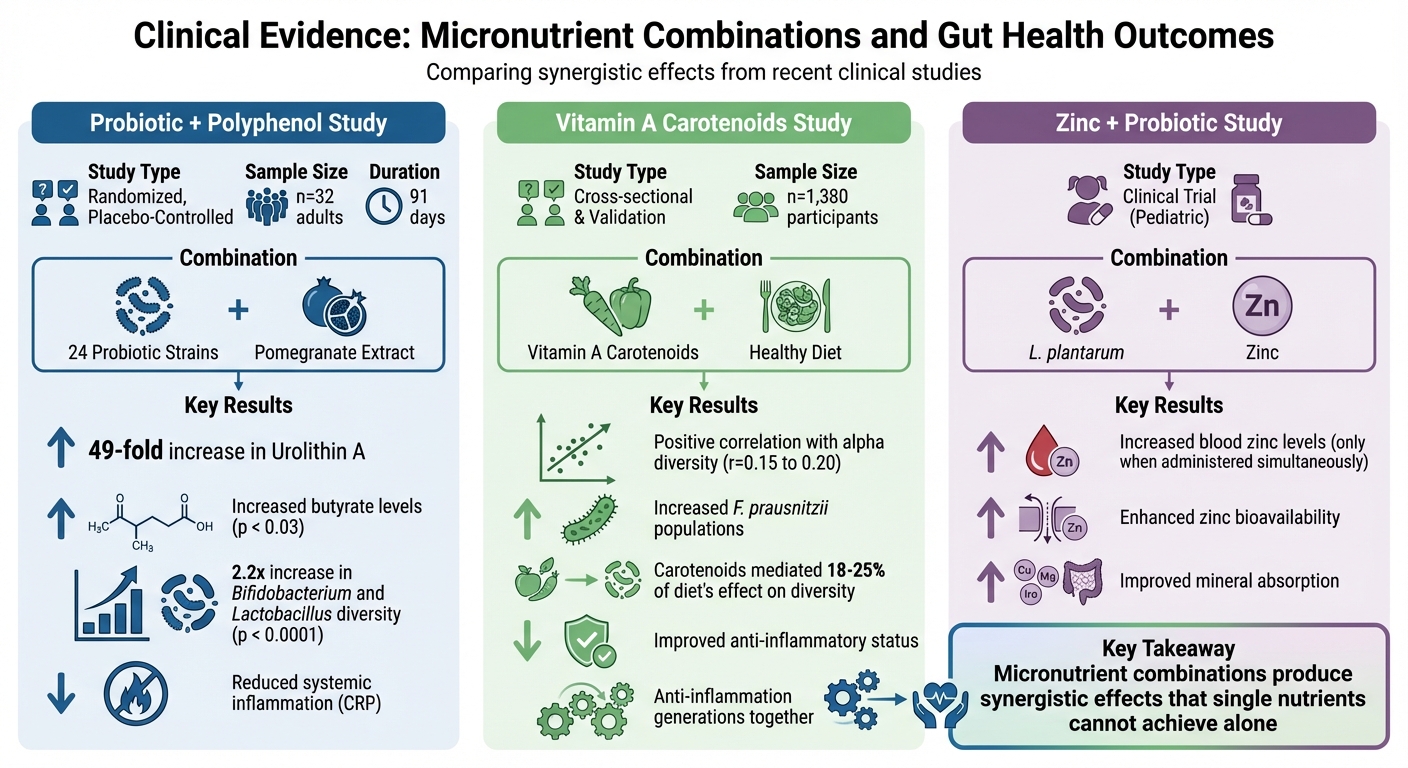
Micronutrient Synergy Effects on Gut Microbiome: Clinical Study Results
Recent research has taken a closer look at the effects of combining micronutrients, using clinical trials to quantify their benefits.
Study Findings Comparison
Clinical trials have consistently shown that specific combinations of micronutrients can improve gut health. One example is a study conducted by researchers from Seed Health, Inc. and Harvard Medical School, published in August 2025. This 91-day randomized, placebo-controlled trial involved 32 healthy adults and tested the DS-01 synbiotic, a mix of 53.6 billion AFU multi-species probiotics and 400 mg of Indian pomegranate extract. By the end of the study, participants experienced a 49-fold increase in urinary Urolithin A levels and improved fecal butyrate levels (p < 0.03), particularly among those with lower baseline levels. The synbiotic also increased the alpha-diversity of Bifidobacterium and Lactobacillus species (p < 0.0001) [6].
Another study, published in BMC Medicine in August 2024, examined data from 1,053 individuals in the TwinsUK cohort and 327 women in the ZOE PREDICT-1 study. This research found a positive correlation between serum carotenoids, such as beta-cryptoxanthin and carotene diols, and the Shannon diversity index (r = 0.15 to 0.20, p < 4 × 10⁻⁶). These vitamin A metabolites accounted for up to 25% of the positive effect of a healthy diet on gut microbial diversity [15].
| Study Design | Combination | Microbial Diversity Results | Health Outcomes |
|---|---|---|---|
| Randomized, Placebo-Controlled (n=32) [6] | 24 Probiotic Strains + Pomegranate Extract (Polyphenols) | Increased alpha-diversity of Bifidobacterium and Lactobacillus (p < 0.0001) | 49-fold increase in Urolithin A; increased butyrate; reduced systemic inflammation (CRP) |
| Cross-sectional & Validation (n=1,380) [15] | Vitamin A Carotenoids + Healthy Eating Index (HEI) | Positive correlation with alpha diversity (r=0.15 to 0.20); increased F. prausnitzii | Carotenoids mediated 18-25% of diet's effect on diversity; improved anti-inflammatory status |
| Clinical Trial (Pediatric) [5] | L. plantarum + Zinc | Not specified (focus on bioavailability) | Increased blood zinc levels only when administered simultaneously |
These findings highlight the potential for targeted interventions in gut health.
Clinical Applications
The studies provide actionable insights into how micronutrient combinations can be used effectively. Timing and pairing are especially important. For example, zinc supplementation alone often fails to address deficiencies. However, when paired with Lactobacillus plantarum, blood zinc levels show a significant increase [5]. This approach offers a practical solution for addressing mineral deficiencies through specific probiotic-mineral combinations.
The 2025 trial also showed that an individual's baseline microbiome status plays a critical role in determining their response. Participants with low baseline butyrate levels experienced statistically significant increases, and by day 91, all participants in the synbiotic group gained the ability to convert polyphenols into Urolithin A. In contrast, only 44.4% of the placebo group achieved this capability [6]. These results suggest that combining micronutrients can help restore missing metabolic functions in the gut microbiome, reducing dysbiosis and promoting better gut health overall.
sbb-itb-1bbfe7f
Practical Applications and Future Research
Diet Strategies for Gut Health
Pairing the right foods can work wonders for gut health. For example, combining zinc-rich foods like oysters, beef, and pumpkin seeds with probiotic sources such as yogurt or kimchi can significantly improve zinc absorption. This is supported by findings that Lactobacillus plantarum, when taken alongside zinc supplements, enhances zinc bioavailability dramatically [5].
Similarly, pairing iron supplements with galactooligosaccharides (GOS) - naturally found in legumes or available as supplements - can help curb the iron-induced growth of harmful E. coli [5]. Magnesium, which you can get from nuts, seeds, or leafy greens, plays a key role in activating enzymes that metabolize vitamin D. Without enough magnesium, your body struggles to use vitamin D effectively [5][3].
Polyphenol-rich foods, like pomegranates, grapes, and berries, also deserve a spot on your plate. These foods provide compounds that gut bacteria transform into anti-inflammatory metabolites, such as Urolithin A [6]. Plus, your gut microorganisms are hard at work producing essential B-vitamins like biotin, folate, and riboflavin - accounting for an estimated 40% to 65% of these vitamins [5][3].
What We Still Need to Learn
Despite these advances, there’s still a lot we don’t know. One major hurdle is the lack of standardized protocols for sample collection and data analysis, making it tough to compare findings across studies [16][17]. Cindy D. Davis, PhD, highlights another challenge:
"Duration of intervention needed to elicit long-term or permanent changes in gut microbiome is unknown" [16].
Defining what constitutes a "healthy" gut microbiome remains a hotly debated topic. Researchers also need more in-depth studies to establish cause-and-effect relationships between dietary habits and microbiome changes, rather than just correlations [16][18].
Micronutrient deficiencies are another pressing issue, affecting around two billion people globally - often due to poor nutrient absorption rather than insufficient intake [3]. Professor Patrizia Brigidi from the University of Bologna underscores the potential of personalized solutions:
"Personalized microbiome-based intervention strategies could therefore constitute an innovative tool to counteract micronutrient deficiencies by modulating the gut microbiome toward an eubiotic configuration" [5].
These gaps in understanding are driving efforts to create practical strategies that harness the synergy between micronutrients and gut health.
How Begin Rebirth RE-1™ Supports Microbiome Health

Addressing these research gaps, Begin Rebirth RE-1™ offers a practical solution grounded in recent scientific advancements. This product is designed to reset the gut microbiome using a clinically supported 3-in-1 eubiotic synbiotic that combines prebiotics, probiotics, and postbiotics.
Each serving delivers 500 billion CFU of Human Origin Strains (HOSt™), specifically formulated to restore gut balance quickly. The proprietary Lyosublime™ delivery system ensures that live strains survive the digestive process and are absorbed effectively.
The formulation also includes 4.5 grams of fiber from GOS and inulin, which promote the production of short-chain fatty acids. Clinical studies show that multi-species formulations like this can increase the diversity of beneficial Bifidobacterium and Lactobacillus species by 2.2 times over 91 days [6]. Offered in 7-day, 4-week, and 12-week programs, Begin Rebirth RE-1™ provides a practical and science-backed approach for tackling dysbiosis and boosting overall immune health.
Conclusion
The evidence presented highlights the powerful role of micronutrient synergy in promoting gut health.
Studies reveal that combining micronutrients delivers more pronounced benefits than using them in isolation. This synergy enhances gut microbiome diversity and supports the production of beneficial metabolites. The gut microbiome itself functions as a "metabolic powerhouse", producing 40% to 65% of essential B-vitamins and improving the absorption of key minerals like calcium, magnesium, and iron [5][3].
Clinical trials further demonstrate that multi-species synbiotics significantly improve the diversity of beneficial gut bacteria and promote metabolite production. These formulations notably increase Bifidobacterium and Lactobacillus populations while boosting levels of metabolites like butyrate and Urolithin A, which are associated with reduced inflammation and stronger gut barrier function [1][6]. Multiple studies confirm these synergistic effects across various metabolic pathways.
The main takeaway? Pairing specific micronutrients strategically yields better results. For instance, combining vitamin D with magnesium or probiotics with polyphenols leads to outcomes that single nutrients or strains alone cannot achieve. As Professor Patrizia Brigidi explains:
"The gut microbiome can variously influence the bioavailability of micronutrients, as well as be influenced by micronutrient supplementation, with implications for health even in the long term" [5].
These insights open the door to smarter dietary choices and supplementation strategies. Incorporating nutrient-dense, polyphenol-rich foods alongside targeted supplements can optimize gut health. Begin Rebirth RE-1™ reflects this research, offering a practical, clinically supported solution to restore microbiome balance and enhance beneficial metabolite production through its 7-day, 4-week, and 12-week reset programs.
FAQs
How do certain micronutrient combinations improve gut health?
Micronutrients can work wonders for gut health when combined thoughtfully. This interaction, known as micronutrient synergy, happens when vitamins and minerals team up to support your gut more effectively than they would on their own. Take vitamin A, zinc, and iron, for instance. Together, they encourage the growth of beneficial gut bacteria like Bacteroides while keeping harmful microbes in check. These nutrients play a key role as cofactors for bacterial enzymes, which are essential for maintaining a strong gut barrier and producing short-chain fatty acids.
Another great example is vitamin C, which boosts iron absorption. This not only helps address iron deficiency but also provides vital nutrients for gut microbes, promoting a more diverse and balanced microbiome. Combinations like B-vitamins (B6, B12, folate) paired with selenium and copper are also powerful. They help reduce oxidative stress and strengthen the gut lining, making a significant impact on overall gut health.
Products such as Begin Rebirth RE-1™ take advantage of these principles by blending prebiotics, probiotics, and postbiotics with essential micronutrients. This targeted formula is designed to balance and strengthen the microbiome, restoring gut health, boosting immunity, and addressing dysbiosis - sometimes in as little as 7 days.
How do B-vitamins support the production of short-chain fatty acids in the gut?
B-vitamins are essential players in maintaining gut health, serving as important cofactors for gut microbes. They help gut bacteria break down dietary fibers through enzymatic fermentation, a process that produces short-chain fatty acids (SCFAs). These SCFAs are critical for keeping the gut lining strong, supporting the immune system, and ensuring smooth digestive function.
By boosting microbial activity, B-vitamins contribute to a well-balanced and healthy gut microbiome, which is key to overall health and wellness.
Why does your body need magnesium to activate vitamin D in the gut?
Magnesium plays a critical role as a co-factor for enzymes responsible for converting vitamin D into its active forms. If magnesium levels are too low, your body might find it harder to fully activate vitamin D, potentially reducing its effectiveness.
On top of that, magnesium helps support gut microbes involved in the synthesis of vitamin D. This connection highlights its importance not just for vitamin D activation but also for promoting a balanced gut microbiome.

